Should you take probiotics after antibiotics?

Antibiotics can be very important to help fight off infections and harmful bacteria, but antibiotics can also leave your gut vulnerable by killing off good bacteria alongside the harmful bacteria.
Your gut microbiome is home to trillions of friendly bacteria known as 'gut microbiota' that are fundamental in the digestion and absorption of nutrients, fighting off pathogens and protecting the intestinal barrier. The more diverse your gut microbiome is with different bacterial species, the better. Expert nutritionist Jessica Rose Turnbull, ANutr, BSc, explains how a loss in diversity of bacteria in your gut - known as 'dysbiosis' - can occur when taking antibiotics, and the important role probiotics play in restoring the balance and health of your gut and your overall health.
Why take a probiotic after antibiotics?
Antibiotics can disrupt the balance of your beneficial gut bacteria for up to 2 years post-treatment. Most people don't realise this, but fear not, because probiotics can offset any damage to the gut by restoring the good bacteria. In one study, for example, researchers found that a 14-day probiotic intervention reduced antibiotic-associated disturbances in the gut microbiota. Importantly, research has shown probiotics can prevent and reduce diarrhoea, which is the most common antibiotic-associated symptom, and affects up to 30% of individuals taking antibiotics. In up to 30% of antibiotic-associated diarrhoea cases, the diarrhoea is due to 'C. difficile', a bacterium that can cause an infection of the large intestine that is frequently associated with antibiotic use. Our nutritional therapist, Isabelle Nunn, who was a practising pharmacist for over 10 years, answers the 7 most commonly asked questions about probiotics.
Not sure what your body needs? Create your Diet Profile.
Diarrhoea is one sign of an unhealthy gut. Discover 5 more signs of bad gut health and learn from our nutritionists about why you should improve your gut health. You may also enjoy reading about what your poo says about your health.
How long does it take the immune system to recover after antibiotics?
Around 70% of your immune system is located in your gut, so dysbiosis of your gut microbiota through the use of antibiotics can affect your ability to fight off viral and bacterial infections. In these instances, probiotics may be able to restore your gut microbiota and boost your immune system as a result.
In general, research suggests that disruption to the gut microbiota following a short course of antibiotics generally lasts between 6 weeks to 6 months, but the loss of some species can remain even after this time. Studies show promising results on the immune system from taking probiotics after taking antiobiotics. For example, one study showed that a seven-month intervention using Lactobacillus rhamnosus GG was able to prevent certain bacterial infections for the following 3 years which in turn correlated with reduced antibiotic use. Additionally, another study using a multi-strain Lactobacillus protocol for 12 weeks, observed increasing levels of antibodies in the gut, demonstrating benefits to the immune system. Your diet also plays a vital role in supporting your immunity - discover the best '8 immunity boosting foods'.
Gut Health Bundle

What should I eat when taking antibiotics?
A very important dietary consideration when it comes to your gut microbiome is fibre intake - fibre is essential in your diet. Dietary fibre can be defined as:
- Soluble fibre, which is fermented by gut bacteria;
- Insoluble fibre, which can improve digestion by slowing down the transit of food through the digestive tract.
Dietary fibre that assists with the survival of beneficial bacteria in the gut microbiome is referred to as 'prebiotics'. Prebiotics are naturally present in plant foods, including asparagus, sugar beet, garlic, chicory, onion, Jerusalem artichoke and wheat. Learn more in 'What are prebiotics' and discover the difference between prebiotics and fibre.
The use of antibiotics has been shown to deplete micronutrients, specifically Vitamin K, which assists with the blood clotting process, and Vitamin B12, which is integral for the brain and nervous system. The good news is that probiotics have been shown to provide positive impacts on the status of certain micronutrients (Vitamin B12, Calcium, Folate, Iron and Zinc), demonstrating their importance when taking antibiotics. Learn more about the best and worst foods for gut health.
Having sufficient fibre in your diet is vital for overall gut health and regular bowel movements. However, high-fibre foods can produce more gas in the gut, which can translate into smelly farts. Our expert nutritionists explain how to know if you need a fibre supplement. You may also enjoy reading 'What do your farts say about your health?'.
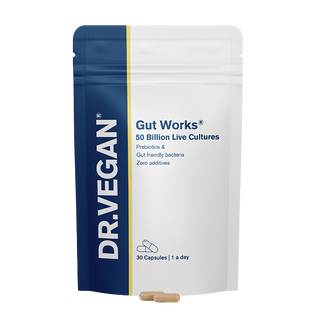
Best probiotic to take after antibiotics
The award-winning Gut Works® is a prebiotic and probiotic with 50 billion live cultures and 6 clinically studied strains, including Lactobacillus Acidophilus, Lactobacillus Rhamnosus, Bifidobacterium and Streptococcus. Crucially, Gut Works® also includes prebiotics to stimulate the growth of your beneficial gut bacteria. A customer survey by DR.VEGAN® showed Gut Works® to be 3x more effective than other probiotic supplements.*
How long after taking antibiotics should you take probiotics?
For best results, you should wait 1 or 2 hours after taking antibiotics before taking your probiotic, and continue take a probiotic for several weeks once your antibiotic treatment has finished. Ensure you take Gut Works® at least 20 minutes before or after any hot drinks.
Discover our range of award-winning vegan supplements and probiotics.
By: Jessica Rose Turnbull, ANutr, BSc. Jessica is a Nutritionist (ANutr, BSc) specialising in plant-based nutrition and gut health.
Gut Works
*Based on a UK survey conducted by DR.VEGAN® of 246 customers, nationally representative, during August & September 2022. All customer survey findings reflect our own efforts and have not been influenced or verified by any external organisations or third-party entities.
You may also enjoy reading:
- Why your gut is your second brain
- How your gut and vagina are linked
- The gut-skin axis
- Estrobolome, your gut & oestrogen
- The 'Gut-Hormone Connection' explained
- How your gut and vagina are linked
- The impact of your gut on your heart
References
- Jernberg, C., Löfmark, S., Edlund, C. and Jansson, J.K. (2007) 'Long-term ecological impacts of antibiotic administration on the human intestinal microbiota', The ISME Journal, 1(1), pp. 56-66 Available at: https://doi.org/10.1038/ismej.2007.3.
- Kabbani, T.A., Pallav, K., Dowd, S.E., Villafuerte-Galvez, J., Vanga, R.R., Castillo, N.E., Hansen, J., Dennis, M., Leffler, D.A. and Kelly, C.P. (2017) 'Prospective randomized controlled study on the effects of Saccharomyces boulardii CNCM I-745 and amoxicillin-clavulanate or the combination on the gut microbiota of healthy volunteers', Gut microbes, 8(1), pp. 17-32 Available at: https:// doi.org/10.1080/19490976.2016.1267890.
- Shapovalova, M.M., Budnevsky, A.V., Kravchenko, A.Y., Drobysheva, E.S. and Ovsyannikov, E.S. (2018) 'Pathogenesis, Actual Aspects Of Prevention And Treatment Of The Antibiotic Associated Diarrhoea', Arhivʺ Vnutrennej Mediciny, 8(6), pp. 424-429 Available at: https://doi.org/ 10.20514/2226-6704-2018-8-6-424-429.
- Goodman, C., Keating, G., Georgousopoulou, E., Hespe, C. and Levett, K. (2021) 'Probiotics for the prevention of antibiotic-associated diarrhoea: a systematic review and meta-analysis', BMJ open, 11(8), pp. e043054 Available at: https://doi.org/10.1136/ bmjopen-2020-043054.
- Palleja, A., Mikkelsen, K.H., Forslund, S.K., Kashani, A., Allin, K.H., Nielsen, T., Hansen, T.H., Liang, S., Feng, Q., Zhang, C., Pyl, P.T., Coelho, L.P., Yang, H., Wang, J., Typas, A., Nielsen, M.F., Nielsen, H.B., Bork, P., Wang, J., Vilsbøll, T., Hansen, T., Knop, F.K., Arumugam, M. and Pedersen, O. (2018) 'Recovery of gut microbiota of healthy adults following antibiotic exposure', Nature microbiology, 3(11), pp. 1255-1265 Available at: https://doi.org/10.1038/s41564-018-0257-9.
- Korpela, K., Salonen, A., Virta, L.J., Kumpu, M., Kekkonen, R.A. and De Vos, W.M. (2016) 'Lactobacillus rhamnosus GG Intake Modifies Preschool Children's Intestinal Microbiota, Alleviates Penicillin-Associated Changes, and Reduces Antibiotic Use', PLoS ONE, 11(4), pp. e0154012 Available at: https://doi.org/10.1371/journal.pone.0154012.
- Zhang, H., Yeh, C., Jin, Z., Ding, L., Liu, B.Y., Zhang, L. and Dannelly, H.K. (2018) 'Prospective study of probiotic supplementation results in immune stimulation and improvement of upper respiratory infection rate', Synthetic and Systems Biotechnology, 3(2), pp. 113-120 Available at: https://doi.org/10.1016/j.synbio.2018.03.001.
- Montenero, A.S. (1980) 'Drugs producing vitamin deficiencies', Acta vitaminologica et enzymologica, 2(1-2), pp. 27-45 Available at: https://www.ncbi.nlm.nih.gov/pubmed/7211625.
- Barkhidarian, B., Roldos, L., Iskandar, M.M., Saedisomeolia, A. and Kubow, S. (2021) 'Probiotic Supplementation and Micronutrient Status in Healthy Subjects: A Systematic Review of Clinical Trials', Nutrients, 13 (9), pp. 3001 Available at: https://doi.org/10.3390/nu13093001.
Want to hear more from our nutritionists? Sign up to our email newsletter for insights and exclusive offers: